Soap Notes Meaning
Soap Notes Meaning - Occupational therapy soap note. Soap notes counseling what are soap notes Vet tech student vet tech school veterinary technician
Soap Notes Meaning
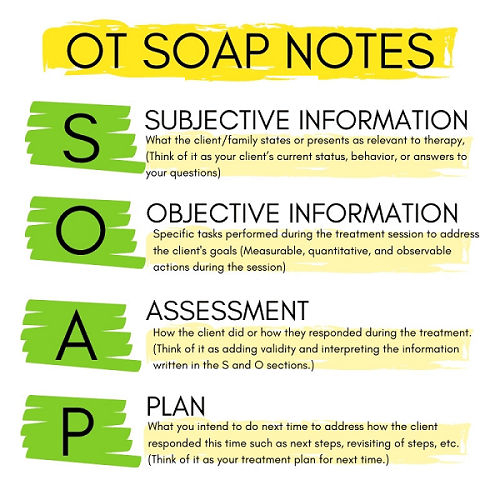
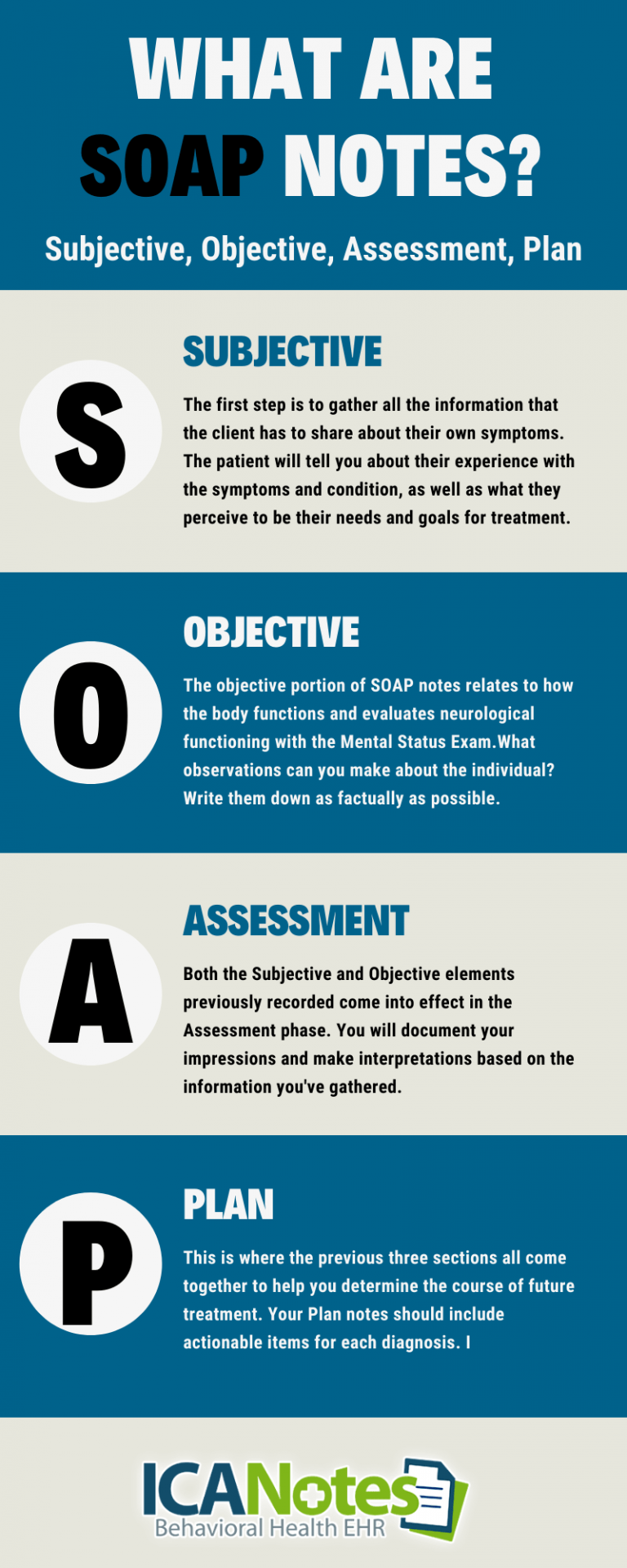
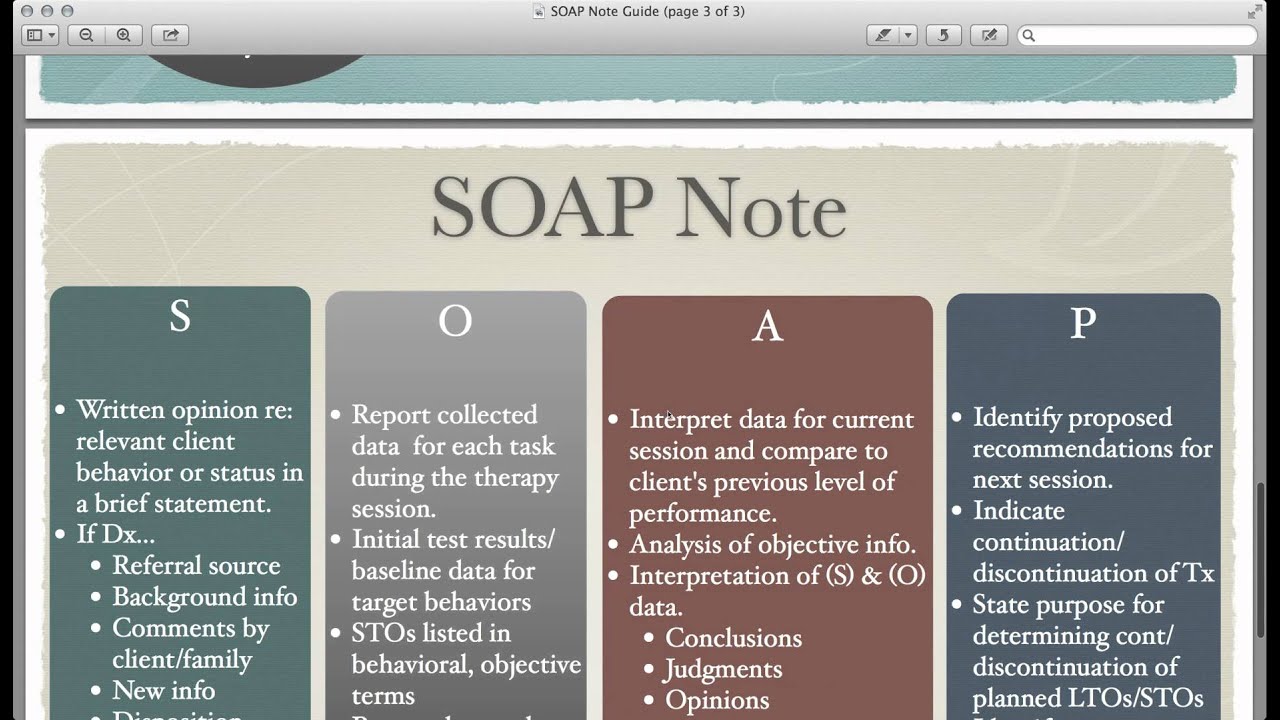
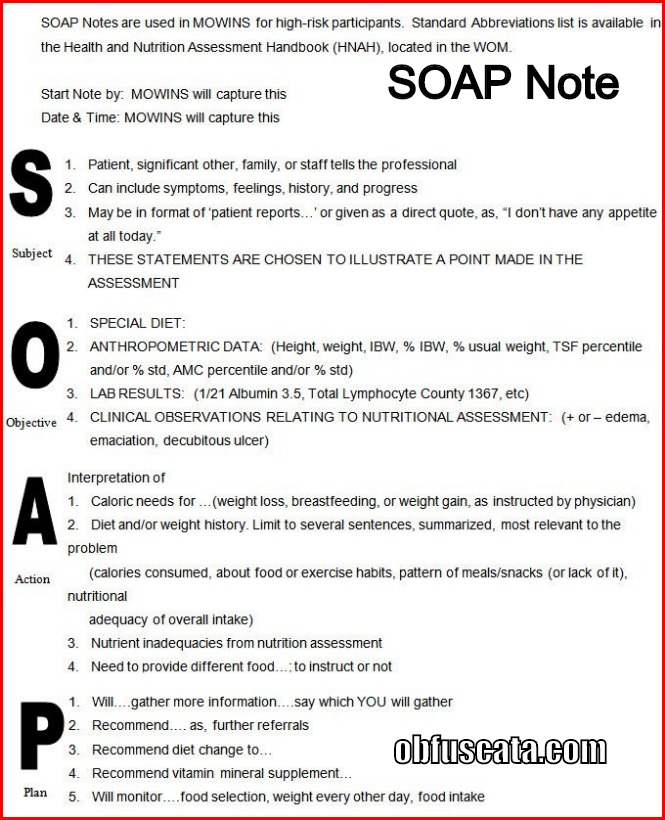
Web Dec 3 2020 nbsp 0183 32 SOAP is an acronym for the 4 sections or headings that each progress note contains Subjective Where a client s subjective experiences feelings or perspectives are recorded This might include subjective information from a patient s guardian or someone else involved in their care ;What are SOAP notes? By: Kunal Sindhu, MD Mastering SOAP notes takes some work, but they’re an essential tool for documenting and communicating patient information. Ineffective communication is one of “the most common attributable causes of sentinel events,” according to an article in the Journal of Patient Safety.
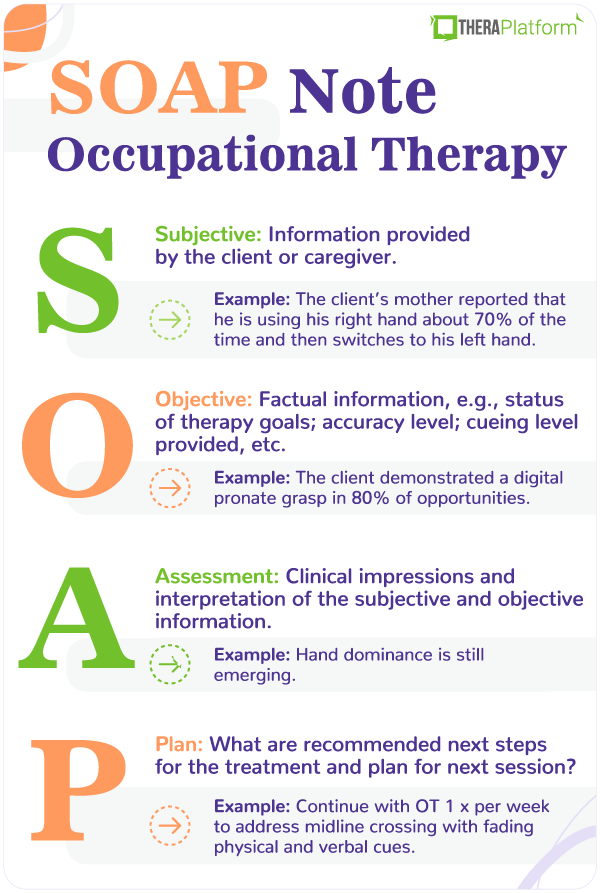
Occupational Therapy SOAP Note

Pharmacy Times Continuing Education Krikiljanganpak
Soap Notes MeaningThe SOAP note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare providers to write out notes in a patient's chart, along with other common formats, such as the admission note. Web Aug 29 2022 nbsp 0183 32 The Subjective Objective Assessment and Plan SOAP note is an acronym representing a widely used method of documentation for healthcare providers The SOAP note is a way for healthcare workers to document in a structured and organized way
Gallery for Soap Notes Meaning

Occupational Therapy Soap Note Template

SOAP Notes Counseling What Are SOAP Notes

Pin On Clinical Documentation

Vet Tech Student Vet Tech School Veterinary Technician
Tips For Writing Better Mental Health SOAP Notes Updated 2021
How To Write A Soap Note For Mental Health How To Write SOAP Notes

Restart Behavioral Health And Wellness
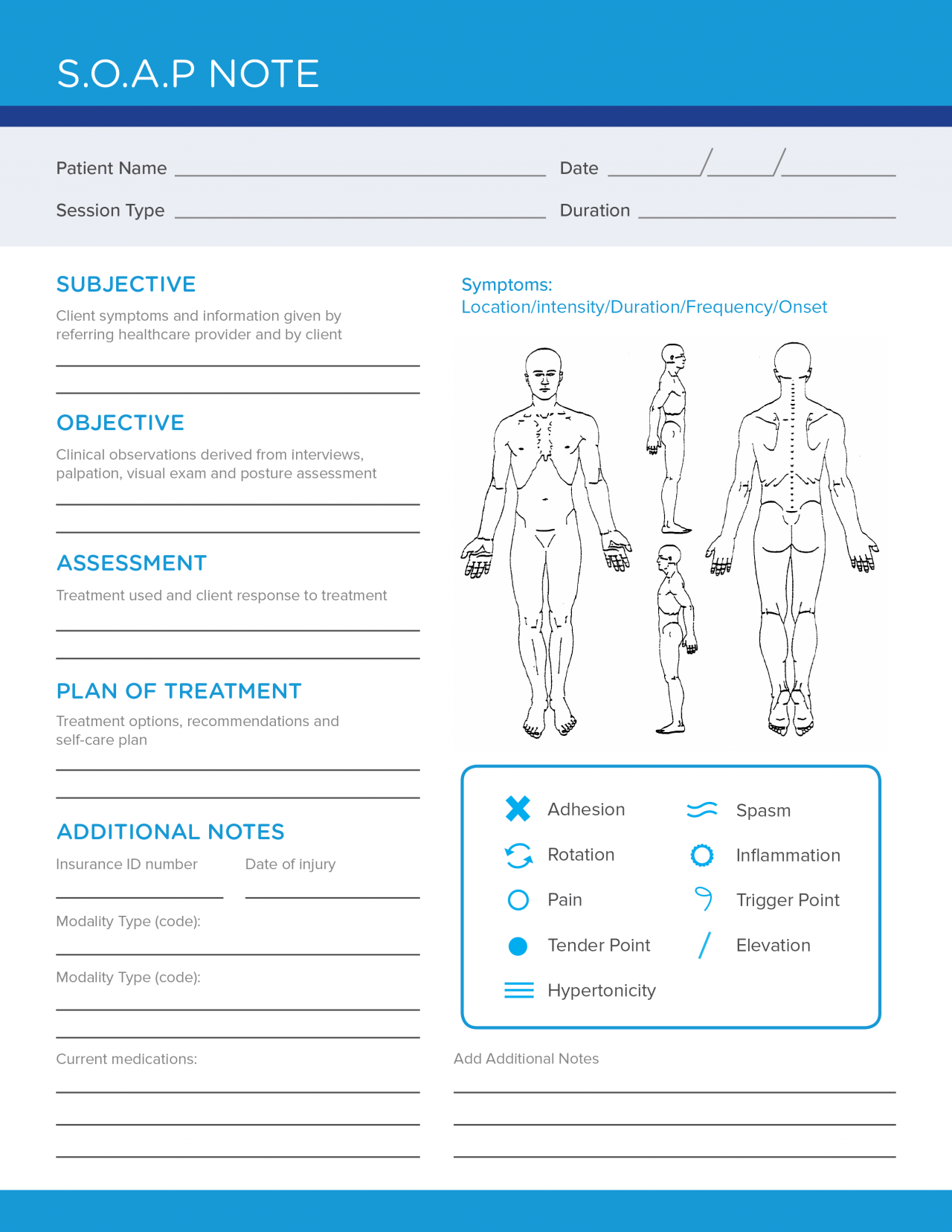
Printable Soap Note Template Pdf Printable Blank World

Counseling DAP Notes A Collection Of Other Ideas To Try Counselor Examples And Note
Nursing Cheat Sheet Template DocTemplates